Researchers decode Spanish flu
Manitoba scientists hope study will help fight future pandemics
Advertisement
Read this article for free:
or
Already have an account? Log in here »
To continue reading, please subscribe:
Monthly Digital Subscription
$19 $0 for the first 4 weeks*
- Enjoy unlimited reading on winnipegfreepress.com
- Read the E-Edition, our digital replica newspaper
- Access News Break, our award-winning app
- Play interactive puzzles
*No charge for 4 weeks then billed as $19 every four weeks (new subscribers and qualified returning subscribers only). Cancel anytime.
Read unlimited articles for free today:
or
Already have an account? Log in here »
Hey there, time traveller!
This article was published 14/08/2018 (2078 days ago), so information in it may no longer be current.
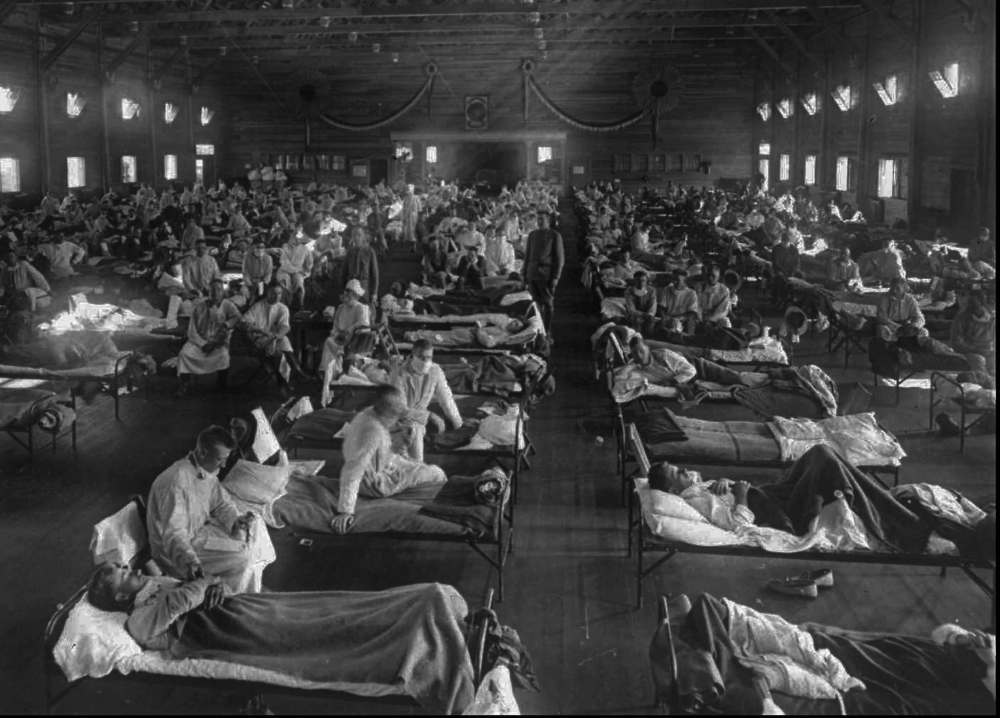
One hundred years after the Spanish flu killed between 50 and 100 million people worldwide, a team of Manitoba researchers has discovered what made the virus so much deadlier than other types of flu.
In a study published this month in EBioMedicine, the researchers did a quantitative analysis of proteins in lung cells, some of which had been infected by the flu virus while others hadn’t been. They then compared both sets of cells, and found dozens of cellular proteins in the Spanish flu sample had their levels boosted or decreased significantly, including many proteins which hadn’t previously been thought affected by the Spanish flu.
By singling out those cellular proteins affected by the virus, the researchers hope their work will help provide a road map in developing effective vaccines, not only against the Spanish flu, but also more recent strains that affect the world today.
“Ultimately, this is going to help all researchers to better understand what makes a bad pandemic flu virus so deadly, so that we can create better medicines to combat it,” said Kevin Coombs, a professor of medical microbiology at the University of Manitoba’s Max Rady College of Medicine.
Coombs co-authored the study with doctors Darwyn Kobasa and Charlene Ranadheera of the Public Health Agency of Canada, the organization that runs the National Microbiology Laboratories in Winnipeg, the only place in Canada where the virus is available for study. Other groups in Canada are doing similar research, but the lab being in Winnipeg made the study possible, Coombs said.
The study is the last in a series of six the researchers have done over the past six years. The experimental work for the most recent study took about a year, and the analysis took about two more. Using the university’s mass spectrometry facilities, the group was able to measure the regulation of those cellular proteins, and managed to compare how the Spanish flu affected cellular pathways as opposed to less deadly flus.
What they found was that the Spanish flu virus turns on a key cellular regulatory pathway more than other flu viruses tested, which leads to more significant impact on the host. In 2009, when the H1N1 pandemic flu broke, a similar phenomenon occurred, Coombs said. In both the case of the 1918 flu and the 2009 one, he added, it isn’t the virus that kills people, but the body’s response. By triggering the pathway to go into overdrive, to put it simply, the body responds at a level of intensity that could kill those infected. A high inflammatory response often leads to a massive release of fluid, which can then enter lung cells and essentially drown the body from the inside, Coombs said.
“It’s analogous to anaphylactic shock,” he said. “It causes the body to have an abnormally strong response against the virus.”
While the Spanish flu outbreak occurred a century ago, Coombs says it’s important to note that the flu has been affecting humans for about 600 years. And although the Spanish flu was “the single worst infectious disease event in human history,” humans still die from flu viruses each year. To make matters more difficult for researchers, the viral proteins related to flu viruses mutate rather rapidly, and vaccines change in accordance with the mutations.
That’s why this research has the potential to make a difference, Coombs said. Cellular proteins don’t mutate anywhere near as much as viral ones do, so to isolate cellular material used by flu viruses provides new insight into potential vaccines.
“If we can identify cellular proteins the virus absolutely requires to carry out disease, and if those proteins aren’t important to the cell, then we can target those instead of the virus, and thereby get closer to a universal vaccine,” Coombs said.
Next steps for research include analyzing the proteins qualitatively, looking at how the proteins “talk to each other,” Coombs said. As well, future studies will test how animal models respond to changes to the proteins found to be involved in the Spanish flu (this round of research was all done in test-tubes).
“Better understanding host cell responses to the flu may be the only way to stay ahead in the microbial ‘arms race’ in order to prevent re-emergence of this and of other deadly flu viruses,” Coombs said.
ben.waldman@freepress.mb.ca

Ben Waldman
Reporter
Ben Waldman covers a little bit of everything for the Free Press.
History
Updated on Wednesday, August 15, 2018 6:40 AM CDT: Adds photo
Updated on Wednesday, August 15, 2018 11:58 AM CDT: corrects hyphen use in number


